Do Babies Really Have Confused Between Breast Bottle
Abstract
Nipple confusion, an infant's difficulty with or preference for one feeding mechanism over another after exposure to artificial nipple(s), has been widely debated. This is in part due to conflicting statements, one by the American Academy of Pediatrics in 2005 suggesting that infants should be given a pacifier to protect against Sudden Infant Death Syndrome, and the other by the World Health Organization in 2009 stating that breastfeeding infants should never be given artificial nipples. Despite the limited and inconsistent evidence, nipple confusion is widely believed by practitioners. Therefore, there is a unique opportunity to examine the evidence surrounding nipple confusion by assessing the research that supports/refutes that bottle feeding/pacifier use impedes breastfeeding efficacy/success/duration. This review examined 14 articles supporting and refuting nipple confusion. These articles were reviewed using the Johns Hopkins Nursing Evidence-Based Practice Rating Scale. Based on our review, we have found emerging evidence to suggest the presence of nipple confusion only as it relates to bottle usage and found very little evidence to support nipple confusion with regards to pacifier use. The primary difficulty in conclusively studying nipple confusion is establishing causality, namely determining whether bottles'/pacifiers' nipples are causing infants to refuse the breast or whether they are simply markers of other maternal/infant characteristics. Future research should focus on prospectively examining the causality of nipple confusion.
What is nipple confusion?
The ambiguity regarding the phrase 'nipple confusion' is evidenced in even the definition of the term, with little agreement among researchers whom have attempted to define it. The most widely cited definition in the literature is by Neifert et al. 1 who divide nipple confusion into two types, A and B. Type A describes a neonate's difficulty in establishing the necessary oral configuration, latching technique and sucking pattern to extract milk from the breast after exposure to an artificial teat1; whereas Type B refers to older infants who have already established breastfeeding but begin to refuse the breast or prefer the bottle.1 Dowling and Thanattherakul2 define nipple confusion more specifically by stating that nipple confusion is the infant's response to the various mechanical and flow characteristics afforded by an artificial nipple compared with the breast, which in turn causes the infant to prefer one feeding mechanism over the other. Based on these previous definitions, we will broadly define nipple confusion as an infant's difficulty with or preference for one feeding mechanism over another after exposure to artificial nipple(s).
Who is confused?
With an increasing focus on the importance of breastfeeding, the World Health Organization released a Baby Friendly Hospital Initiative that outlined 10 steps for successful breastfeeding. These steps aim to support optimal infant feeding by promoting exclusive breastfeeding from birth to 6 months.3 Although many of these steps have evidence to support their implementation, step nine, 'Give no artificial teats or pacifiers to breastfeeding infants', has been widely debated.3 Adding to the confusion is the conflicting suggestion by the American Academy of Pediatrics, who recommends pacifiers be provided once breastfeeding has been initiated as a method to prevent Sudden Infant Death Syndrome.4 This conflicting information has left parents and health-care providers at an impasse, with little clarity on the subject.
Parents considering breastfeeding are not the only ones confused about this critical issue. Pediatricians, neonatal nurses and other health-care providers are also unsure about best practice given the limited and conflicting evidence surrounding nipple confusion. In one study, nurses in a level II Neonatal Intensive Care Unit, postpartum nurses and pediatricians were asked whether they believed that frequent bottle feeds could result in nipple confusion in neonates based on the Type A definition by Neifert et al. 1 They found mixed results: 15% of level II nurses, 44.4% of postpartum nurses and 56.2% of pediatricians believed that frequent bottle feeds could cause nipple confusion. The same cohort was asked if even one bottle feed could result in nipple confusion and 2.4% of level II Neonatal Intensive Care Unit nurses, 17.4% of postpartum nurses and 6.2% of pediatricians responded yes.5 Similarly, Cloherty et al. 6 found that nipple confusion is widely believed by practitioners and affects their daily practice, despite the limited and conflicting evidence. Given these discrepancies in clinical opinion and practice, review of the evidence surrounding this theory is necessary to elucidate and guide clinical practice.
There exists a sharp divide in the literature between those who believe that nipple confusion exists and those who do not. Numerous studies have looked directly and indirectly at the effect of pacifiers or bottle-feeding on subsequent breastfeeding (efficacy/success/duration). These studies, and their evidence, will be examined in-depth within this review paper in an effort to promote evidence-based practice across professions in infant feeding.
Method
Research studies were found through a comprehensive search using Northeastern University's Scholar OneSearch with the keywords 'nipple+confusion'. This search produced 235 results. Narrowing the years of studies from 1990 to 2014 yielded 227 studies. Inclusion criteria at this level included either specifically measuring nipple confusion or containing a measure of breastfeeding rate/exclusivity. Of these, 16 were excluded for being non-research articles (that is, letters to the editor), two books were excluded, two articles were excluded for not being available in English and one video was excluded. In addition, 206 studies were excluded for being irrelevant or duplicate, resulting in 28 studies that were systematically reviewed.
These 28 studies were reviewed for relevance as a novel research article. No reviews or practice statements were included. After an initial review, 14 studies were excluded because breastfeeding rate/exclusivity was not measured in relation to bottle-feeding and/or pacifier use only (including those with aims comparing cup and bottle feeding), and 14 were included. The reference lists of the 14 included studies were systematically reviewed, and 5 additional articles were identified from those references and added to the review based on the aforementioned inclusion criteria. Thus a total of 19 studies were included at this point for review.
These 19 studies were critically evaluated using the Johns Hopkins Nursing Evidence-Based Practice Rating Scale.7 This evidence rating scale was chosen based on its ease of use, relevance to the included studies and comprehensive nature. This rating scale has been used to review evidence-based practice in the nursing field.8, 9 Using this rating scale, each article was given a level rating of I to V for strength of the evidence and a letter rating (A to C) for quality of evidence. Only studies that rated I to III for strength and A or B for quality were included in the final review. Thus 14 studies were included in the final review.
These 14 studies were further parsed to assess the evidence that supports and refutes bottle nipple confusion and pacifier nipple confusion and their influence on breastfeeding efficacy/success/duration. 'Bottle nipple confusion' is used to describe the effect that bottle-feeding has on nipple confusion. That is, the hypothesis that the experience of feeding from a bottle and exposure to the artificial teat will cause the infant to refuse the breast. 'Pacifier nipple confusion' is used to describe the effect pacifier use has on nipple confusion; the hypothesis that giving an infant a pacifier will cause the infant to refuse the breast during breastfeeding, as a result of the exposure to an artificial nipple.
Bottle nipple confusion
We identified six studies investigating bottle nipple confusion. Of these studies, two reported that there was no evidence for nipple confusion and four found evidence to support the phenomenon of nipple confusion (see Figure 1 and Table 1). However, more in-depth and prospective research still needs to be completed examining nipple confusion and bottle usage.
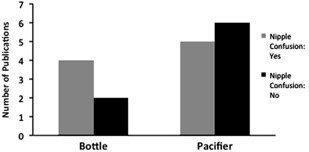
The number of publications reviewed for bottle and pacifier nipple confusion that either supported (gray) or refuted (black) the concept of nipple confusion.
Full size image
Full size table
Evidence against bottle nipple confusion
One of the nipple confusion hypotheses is that infants are unable to adapt to the different sucking mechanisms necessary to switch between breast and bottle. Moral et al. 10 examined the mechanics of sucking between bottle-feeding and breastfeeding infants. This cross-sectional study included infants who were exclusively breastfeeding, exclusively bottle-feeding and mixed feedings (both bottle and breast) across the following age groups: newborn babies (21 to 28 days) and older infants (3 to 5 months). The primary outcome measure was the number of sucks per minute and suck was counted by direct observation of the movements of the jaw. Infants who were exclusively bottle-fed demonstrated fewer sucks than infants who were breastfeeding but with the same number of pauses, although these pauses were of longer duration. In the mixed feeding group, bottle-feeding compared with breastfeeding showed the same number of sucks but fewer and shorter pauses, both at 21 to 28 days and at 3 to 5 months. In sum, this study revealed differences in nutritive suck patterns in exclusively breast-fed infants compared with exclusively bottle-fed infants. However, infants who were fed both by breast and bottle displayed both types of suck patterns when learning to feed, which indicates that the infants ultimately adopted their own effective pattern to either bottle or breast, thereby refuting the hypothesis of nipple confusion.10 It is important to note that this study did not examine the initial 2 weeks following birth, where 'nipple confusion' would likely have the largest impact.
Another study that did not find evidence of bottle nipple confusion is by Schubiger et al. 11 In this study, infants were randomized to either a 'UNICEF' group, where infants were restricted from fluid supplements, bottles and pacifiers during the first 5 days of life, or a standard group with conventional practices, and both groups were encouraged to breastfeed. There were no differences between the two groups in breastfeeding frequency or duration at day 5 or subsequently at 2, 4 and 6 months of age.11 This study provides evidence that exposure to an artificial nipple, either by bottle or pacifier, did not affect breastfeeding frequency or duration. It is also important to note that the infants studied were only restricted from pacifiers and bottles for the first 5 days of life; whether restriction for a longer time period would have produced different results remains to be seen.
Evidence supporting bottle nipple confusion
Overall, four studies in this systematic review provided evidence to support bottle nipple confusion. Two studies reported questionnaire data examining mother–infant feeding characteristics. Hla et al. 12 mailed surveys to women who delivered an infant in Hawaii during a 3-month time period in 1989 and found that shorter breastfeeding duration was associated with the introduction of formula before 6 months of age, suggesting an effect between the introduction of the bottle and breastfeeding. Interestingly, this study also revealed that those who reported problems with breastfeeding were at the highest risk for breastfeeding cessation.12 The second study was completed using a structured interview of mothers of infants aged <12 months.13 Infants were parsed into one of the following categories: exclusive breastfeeding, predominant breastfeeding, complementary breastfeeding, or weaning. The authors found that infants who were bottle-fed were 26 times more likely to be weaning than those not bottle-fed. However, this study offers minimal insight into how the different categories of breastfeeding influence subsequent weaning or any causality related to nipple confusion. The nature of the categories themselves suggests that infants may be bottle-fed because they are, in fact, being weaned from the breast, which could be due to a number of reasons, including mother returning to work or difficulty breastfeeding, among others.
Both Righard14 and Kliethermes et al. 15 found that infants who receive bottle supplementation breastfeed less. The study by Righard14 found that infants who were identified as having trouble breastfeeding were less likely to continue to breastfeed if supplemental bottles had already been instituted. This suggests that bottle supplementation, in addition to the breastfeeding challenges, increased the likelihood of breastfeeding cessation. It is important to note that this study does not confirm or deny the presence of nipple confusion, as these infants already demonstrated difficulty with breastfeeding. Kliethermes et al. 15 were the only group reviewed to examine preterm infants and alternative supplementation related to bottle-feeding and found that infants who received nutrition supplementation via a nasogastric tube had a higher likelihood of breastfeeding at multiple time points (discharge and 3 days/3 months/6 months postdischarge) compared with those given supplementation via a bottle. The authors hypothesized that an imprinting process occurs, although no experimental evidence was presented to support or deny these statements.4, 16 In claims similar to that of Neifert et al.,1 the authors also hypothesized that the instant gratification of bottle-feeding could cause the infant to prefer the bottle over the breast,1, 4 as the bottle nipple releases milk sooner than the breast, which can often take a few minutes for the let-down reflex to release the milk.
Although the research presented on bottle nipple confusion represents the current published evidence, this evidence does not clearly address the underlying causal relationship between the use of bottles and nipple confusion. More research needs to be completed focusing on identifying the underlying mechanisms as well as the causality.
Pacifier nipple confusion
We identified 10 studies investigating pacifier use on exclusivity or duration of breastfeeding. Of these studies, four found evidence to support the phenomenon of nipple confusion and six did not (see Figure 1; Table 1).
Evidence supporting pacifier nipple confusion
Three studies provided evidence based on the hypothesis that pacifier use would shorten overall duration of breastfeeding.17, 18, 19 Barros et al.,17 examined the relation between pacifier use at 1-month old and breastfeeding duration from 1 to 6 months. They found that weaning was significantly related to pacifier use at 1 month and that these infants were three times more likely to be weaned at 6 months of age.17 Another study examining pacifier use at 1 month and breastfeeding at 6 months found similar results; they reported that full-time pacifier users at 1-month old were four times as likely to stop breastfeeding by 6 months, compared with infants who did not use a pacifier.18 The authors concluded that pacifier use seems to contribute to earlier weaning in a group of women who are uncomfortable with breastfeeding; however, pacifiers do not seem to affect breastfeeding duration in self-confident mothers. Thus, pacifiers might be seen as a contributing factor rather than the cause of early breastfeeding termination.18 Finally, a cross-sectional study interviewed mothers of infants <12 months and found that the interruption of exclusive breastfeeding was associated with the following variables: older age of the infant, pacifier use, and lower maternal education level.19 In all of these studies, it was somewhat unclear whether pacifier use was causally related to breastfeeding cessation, or whether it was simply a marker of breastfeeding difficulties present in either the infant or the mother. The results of these studies also suggest that pacifier use could be an indicator of breastfeeding termination and perhaps does not lead to the infant developing nipple confusion.
Howard et al. 20 attempted to determine causality of pacifier nipple confusion with a randomized clinical trial involving four groups: bottle and early pacifier, bottle and late pacifier, cup and early pacifier, and cup and late pacifier. The early pacifier groups were instructed to introduce the pacifier as soon as possible and the late pacifier groups were instructed to introduce the pacifier in the infant's fifth week of life. Breastfeeding duration was categorized as exclusive (only breast milk), full (infrequent use of water, juice or ritualistic feeds) or overall (the length of time infants received any breast feedings). The study showed that, at 4 weeks postpartum, early pacifier use caused a significant decline in the number of infants exclusively breastfed but did not affect full or overall breastfeeding compared with late pacifier use. Interestingly, pacifier use was not the most significant predictor of breastfeeding duration, the receipt of supplemental feedings, regardless of method was, and there were no significant effects of pacifiers on breastfeeding frequency in the first 6 months postpartum.20 Thus, while early pacifier use affected the exclusivity of breastfeeding, it did not affect the overall duration that infants were breastfed. This result again calls into question whether pacifier use is indicative of nipple confusion or a marker of other infant or maternal characteristics/decisions that influence feeding.
Evidence against pacifier nipple confusion
Three studies directly examined the effects of restricting or avoiding pacifiers on breastfeeding outcomes in full-term infants.11, 21, 22 Kair et al. 21 found that restricting pacifier use in one hospital actually resulted in decreased exclusive breastfeeding, increased supplemental formula feeds and increased exclusive formula feeds, the opposite results one might expect if operating under the nipple confusion hypothesis. The authors could not find any significant maternal or infant variables to account for this change. Similarly, Kramer et al. 22 completed a randomized control trial to determine whether pacifier use was related to weaning at 3 months postpartum. Participants were randomly allocated to one of the two counseling interventions. The experimental intervention group (n=140) differed from the control group (n=141) by recommending avoidance of pacifier use and suggesting alternative ways to comfort a crying or fussing infant.22 The authors reported that there was a strong association between pacifier use and weaning by 3 months observationally. However, when data were experimentally analyzed based on random allocation of study groups, there was no association.22 This result strongly suggests that pacifier use may be an indication of breastfeeding problems or a decreased motivation to breastfeed, not of nipple confusion. Finally, as reported previously, Schubiger et al. 11 completed a study with an experimental UNICEF group who were restricted from fluid supplements, bottles and pacifiers during the first 5 days of life.14 Both groups were encouraged to breastfeed. There were no differences between the two groups in breastfeeding frequency or duration at day 5 or subsequently at 2, 4 or 6 months.14 Although it is difficult to discern the potential effect of the artificial nipple of the bottle and pacifier, this study does provide evidence to refute the hypothesis of nipple confusion, as the use or avoidance of artificial nipples did not result in a significant difference in breastfeeding outcome.
One study examined the effect of pacifier use on breastfeeding in preterm infants. This randomized, controlled trial separated infants into four groups: cup/no pacifier, cup/pacifier, bottle/no pacifier, and bottle/pacifier.23 There were no significant differences found between those infants given a pacifier versus those who were not on full breastfeeding, any breastfeeding or prevalence of breastfeeding at 3 and 6 months postdischarge.23 It is important to note that non-compliance was high, as many mothers requested a pacifier for their infant. Even so, this study refutes the hypothesis of nipple confusion in preterm infants, as pacifiers did not affect subsequent breastfeeding, even as far as 6 months postdischarge.
A physiological study of non-nutritive suck also refutes the hypothesis of nipple confusion from the standpoint that infants can modulate their suck output based on the mechanical properties of the pacifier. Zimmerman and Barlow24 presented two pacifiers to infants, one that was seven times stiffer than the other pacifier, and found that the stiffer pacifier significantly degrades suck patterning. This reveals that infants modify their suck output when presented with pacifiers with significantly different mechanical properties. This finding refutes the hypothesis that nipple confusion occurs due to the infant's inability to modulate suck patterning in response to his/her oral environment. However, this study did not specifically measure the infant's ability to modulate non-nutritive suck on an artificial nipple, followed by nutritive suck on the mother's nipple.
Bottle or pacifier nipple confusion or causality
Although this review has shown that the majority of evidence examined supports the concept of bottle nipple confusion and refutes the concept of pacifier nipple confusion, the major limitation in all of these studies is the aspect of causality. The studies presented rarely address the following questions: is nipple confusion its own disorder, purely due to the effects of the alternative nipple? Or, is nipple confusion simply a sign of an infant or mother who is already having difficulty breastfeeding?
Neifert et al. 1 listed numerous infant and maternal risk factors for nipple confusion. These included maternal factors, such as variability in nipples, abnormal breasts, low milk supply, maternal illness and so on, and infant characteristics, including prematurity, birth weight <6 lbs, small or large for gestational age, hypoglycemia and so on.1 For example, it has been suggested that, if infants have not attached correctly, or are in distress during breastfeeding, and one resolves this by giving the infant a bottle, the infant would likely continue this pattern to avoid future distress.16 This calls to question whether nipple confusion is a true phenomenon, or if these mothers and infants are having difficult breastfeeding due to these risk factors.
Experimentally, it is difficult to ascertain whether artificial nipple use is causing limited duration/exclusivity of breastfeeding because of 'nipple confusion' or whether artificial nipple use (bottle or pacifier) serves as a marker of risk factors that could limit breastfeeding, such as those listed above. Very few of the studies found attempted to separate these hypotheses. The overall experimental evidence supporting and refuting the hypothesis of nipple confusion remains mixed due to the difficult task of isolating the effect of 'nipple confusion' rather than artificial nipple use as a marker of weaning.
The evidence presented in this section does not clearly address the underlying causal relationship between pacifier provision and nipple confusion and, instead, solely shows a correlation that may be attributable to another cause.
Summary
Current research suggests that the primary difficulty in conclusively studying the hypothesis of nipple confusion is establishing causality. It is difficult to ascertain whether infants are refusing the breast and preferring the bottle because they are already having trouble breastfeeding or whether they are experiencing nipple confusion. Although a majority of the evidence reviewed suggested the presence of nipple confusion related to bottles, the current state of the research shows that pacifier-related nipple confusion is unlikely. Future research should focus on examining the effects of the artificial nipple and the effects of a pacifier versus bottle, as well as the causality of nipple confusion.
References
- 1
Neifert M, Lawrence R, Seacat J . Nipple confusion: toward a formal definition. J Pediatr 1995; 126 (6): 125–129.
Article Google Scholar
- 2
Dowling D, Thanattherakul W . Nipple confusion, alternative feeding methods, and breast-feeding supplementation: state of the science. Newborn Infant Nurs Rev 2001; 1 (4): 217–223.
Article Google Scholar
- 3
UNICEF/WHO Section 1 Background and Implementation. UNICEF/WHO: Geneva, Switzerland, 2009.
- 4
American Academy of Pediatrics Task Force on Sudden Infant Death S. The changing concept of sudden infant death syndrome: diagnostic coding shifts, controversies regarding the sleeping environment, and new variables to consider in reducing risk Pediatrics 2005; 116 (5): 1245–1255.
Article Google Scholar
- 5
Al-Sahab B, Feldman M, Macpherson A, Ohlsson A, Tamim H . Which method of breastfeeding supplementation is best? The beliefs and practices of paediatricians and nurses. Paediatr Child Health 2010; 15 (7): 427–431.
Article Google Scholar
- 6
Cloherty M, Alexander J, Holloway I, Galvin K, Inch S . The cup-versus-bottle debate: a theme from an ethnographic study of the supplementation of breastfed infants in hospital in the United Kingdom. J Hum Lact 2005; 21: 151–162.
Article Google Scholar
- 7
Newhouse R, Dearholt S, Poe S, Pugh L, White K . The Johns Hopkins Nursing Evidence-Based Practice Rating Scale. The Johns Hopkins Hospital: Baltimore, MD, USA, 2005.
Google Scholar
- 8
Kverno KS, Black BS, Nolan MT, Rabins PV . Research on treating neuropsychiatric symptoms of advanced dementia with non-pharmacological strategies, 1998–2008: a systematic literature review. Int Psychogeriatr 2009; 21 (5): 825–843.
Article Google Scholar
- 9
Grant MS, Jenkins LS . Communication education for pre-licensure nursing students: literature review 2002–2013. Nurse Educ Today 2014; 13: 1375–1381.
Article Google Scholar
- 10
Moral A, Bolibar I, Martinez-Barba C, Moral A, Rios J, Sebastia G et al. Mechanics of sucking: comparison between bottle feeding and breastfeeding. BMC Pediatr 2010; 10: 6.
Article Google Scholar
- 11
Schubiger G, Schwarz U, Tonz O . UNICEF/WHO baby-friendly hospital initiative: does the use of bottles and pacifiers in the neonatal nursery prevent successful breastfeeding? Eur J Pediatr 1997; 156: 874–877.
CAS Article Google Scholar
- 12
Hla MM, Novotny R, Kieffer EC, Mor J, Thiele M . Early weaning among Japanese women in Hawaii. J Biosoc Sci 2003; 35 (2): 227–241.
Article Google Scholar
- 13
Moimaz SA, Zina LG, Saliba NA, Saliba O . Association between breast-feeding practices and sucking habits: a cross-sectional study of children in their first year of life. J Indian Soc Pedod Prev Dent 2008; 26: 102–106.
Article Google Scholar
- 14
Righard L . Are breastfeeding problems related to incorrect breastfeeding technique and the use of pacifiers and bottles? Birth 1998; 25 (1): 40–44.
CAS Article Google Scholar
- 15
Kliethermes PA, Cross ML, Lanese MG, Johnson KM, Simon SD . Transitioning preterm infants with nasogastric tube supplementation: increased likelihood of breastfeeding. J Obstet Gynecol Neonatal Nurs 1998; 28 (3): 264–273.
Article Google Scholar
- 16
Fisher C, Inch S . Nipple confusion—who is confused? J Pediatr 1996; 129 (1): 174–179.
CAS Article Google Scholar
- 17
Barros FC, Tonioli Filho S, Semer TC, Tomasi E, Victoria CG, Weiderpass E . Use of pacifiers is associated with decreased breast-feeding duration. Pediatrics 1995; 95 (4): 497.
CAS PubMed Google Scholar
- 18
Victora CG, Behague DP, Barros FC, Olinto MTA, Weiderpass E . Pacifier use and short breastfeeding duration: cause, consequence, or coincidence? Pediatrics 1997; 99 (3): 445–453.
CAS Article Google Scholar
- 19
do Nascimento MBR, Reis MAM, Franco SC, Issler H, Ferraro AA, Grisi SJFE . Exclusive breastfeeding in southern brazil: prevalence and associated factors. Breastfeed Med 2010; 5 (2): 79–85.
Article Google Scholar
- 20
Howard CR, Howard FM, Lanphear B, Eberly S, deBlieck EA, Oakes D et al. Randomized clinical trial of pacifier use and bottle-feeding or cupfeeding and their effect on breastfeeding. Pediatrics 2003; 111 (3): 511–518.
Article Google Scholar
- 21
Kair LR, Kenron D, Etheredge K, Jaffe AC, Phillipi CA . Pacifier restriction and exclusive breastfeeding. Pediatrics 2013; 131 (4): e1101–e1107.
Article Google Scholar
- 22
Kramer MS, Barr RG, Dagenais S, Yang H, Jones P, Ciofani L et al. Pacifier use, early weaning, and cry/fuss behavior: a randomized controlled trial. J Am Med Assoc 2001; 286 (3): 322–326.
CAS Article Google Scholar
- 23
Collins CT, Ryan P, Crowther CA, McPhee AJ, Paterson S, Hiller JE . Effect of bottles, cups, and dummies on breast feeding in preterm infants: a randomised controlled trial. BMJ 2004; 329 (7459): 193–198.
Article Google Scholar
- 24
Zimmerman E, Barlow SM . Pacifier stiffness alters the dynamics of the suck central pattern generator. J Neonatal Nurs 2008; 14 (3): 79–86.
Article Google Scholar
Download references
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Zimmerman, E., Thompson, K. Clarifying nipple confusion. J Perinatol 35, 895–899 (2015). https://doi.org/10.1038/jp.2015.83
Download citation
-
Received:
-
Revised:
-
Accepted:
-
Published:
-
Issue Date:
-
DOI : https://doi.org/10.1038/jp.2015.83
Do Babies Really Have Confused Between Breast Bottle
Source: https://www.nature.com/articles/jp201583
0 Response to "Do Babies Really Have Confused Between Breast Bottle"
Postar um comentário